AARP Eye Center
Are We There Yet? Efforts to Balance Long-Term Services and Supports
By Jean Accius, July 25, 2016 10:17 AM
“Marvin L. Dawkins was a 53-year-old AT&T manager when a blocked blood vessel left him paralyzed. It took 11 years, one lawsuit, repeated tangles over Medicaid rules — and a chance meeting on a church van — before he could extract himself from a nursing home outside Baltimore. Now he lives in an apartment with the assistance of an aide, gets out for a job that he says gives him purpose, socializes with new friends and old ones, and revels in his freedom.” — New York Times
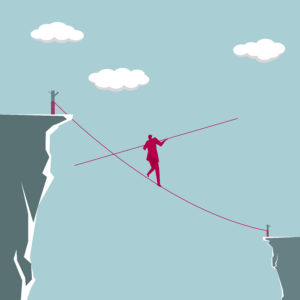
As people age, they want to maintain their independence. They want to have control over their own decisions and receive the assistance that’s both appropriate and allows them to remain in their own homes and communities as long as is reasonably possible. In response, the delivery system for providing long-term services and supports (LTSS) needs to continually adapt to meet the evolving needs of older adults and individuals with disabilities. That is not happening, at least across the board, at a pace that is fast enough to meet growing demand.
Unfortunately, not everyone can gain access to the “right fit” when it comes to LTSS — the kind of fit that took Marvin L. Dawkins, the man in the New York Times report referenced above, 11 years to find. Despite some progress toward flexible LTSS approaches, the LTSS delivery system continues to rely all too heavily on more costly institutional care.
Headed in the right direction
The primary payer of LTSS in the United States is Medicaid, spending $152 billion in fiscal year (FY) 2014. Over the last 30 years, the delivery of LTSS has evolved toward a greater reliance on home- and community-based services (HCBS) as a meaningful alternative to institutional care. In the last decade, LTSS expenditures toward HCBS have consistently increased. In 2013, for the first time, the majority of Medicaid LTSS dollars for all populations went to HCBS.
A recent report from Truven shows that this trend toward HCBS is continuing. In 2014, Medicaid LTSS spending on HCBS for all populations increased from 51.3 percent in 2013 to 53.1 percent in FY 2014. The Centers for Medicare & Medicaid Services projects that by 2020, total LTSS spending for all populations will exceed 63 percent for HCBS relative to institutional care. Such figures indicate a positive trend: tailoring services (that often are more cost effective) to individuals’ needs and preferences.
Trend eludes many
These figures, however, mask substantial spending variations, both by state and by demographic. Because Medicaid is a federal-state partnership administered on the state level, where you live affects your ability to access publicly funded HCBS to meet your LTSS needs.
HCBS is optional under federal Medicaid rules, and states have the flexibility to design their own HCBS offerings and set eligibility criteria at their discretion. While all state Medicaid programs offer options for HCBS as a form of LTSS, access to these benefits can vary significantly by state. Meanwhile, LTSS in institutional settings, such as nursing homes, is a mandatory benefit for all individuals who qualify for Medicaid. This split in optional and mandatory benefits for Medicaid LTSS creates a structural bias toward institutional care and can limit one’s ability to receive services in the setting of one’s choice.
Thus, for older people and adults with physical disabilities, institutional care still accounts for 59 percent of Medicaid LTSS spending. In 2014, Medicaid nursing facility spending was $55.1 billion for older people and adults with physical disabilities, compared to $37.9 billion for HCBS.
Further, there is state variation in the funding of Medicaid HCBS for older adults and individuals with physical disabilities. Those variations range from 12.5 percent to 76.1 percent of all LTSS expenditures. Nine states spent more than 50 percent of their Medicaid LTSS funds on HCBS: Oregon, Minnesota, New Mexico, Washington, Alaska, California, Texas, Colorado and Wisconsin.
While the LTSS delivery system has made significant progress toward offering people more choice and control, it remains too reliant on costly institutional services, especially for older adults and people with physical disabilities. By eliminating the bias in Medicaid LTSS toward institutional care, policymakers could help to align policy with consumer preference — and, at the same time, potentially realize new cost efficiencies and significant returns on investments for government agencies and taxpayers. That way, people like Marvin Dawkins won’t have to fight 11 years to get the service that meets their needs and preferences.
This is part of a series of articles highlighting data for long-term services and supports on AARP Data Explorer.

Jean Accius is vice president of livable communities and long-term services and supports for the AARP Public Policy Institute. He works on Medicaid and long-term care issues.