AARP Hearing Center
Hispanic Adults Get Fewer Wellness Visits in Medicare Advantage Plans
By Keith Lind, September 25, 2019 10:26 AM

This is the fourth in a series of blog posts on Medicare’s Annual Wellness Visit. You can also read a new AARP Public Policy Institute study on the topic.
The Annual Wellness Visit is a free offering for traditional Medicare and Medicare Advantage enrollees created under the Affordable Care Act. At this prevention-focused visit, consumers get appropriate preventive care, discuss with their clinician ways to mitigate health risks, and plan for their future health care needs. Many of the preventive services that wind up happening during and after the Annual Wellness Visit (whether or not they are part of the Annual Wellness Visit itself), such as vaccinations, have been shown to improve patient outcomes and reduce overall Medicare program spending—for example, by limiting the need for more expensive acute care later on.
In short, the benefit has shown positive outcomes. Yet in spite of the Annual Wellness Visit’s no-cost price tag, not all groups are benefitting equally, our recent research finds.
Annual Wellness Visit: Who’s Using It?
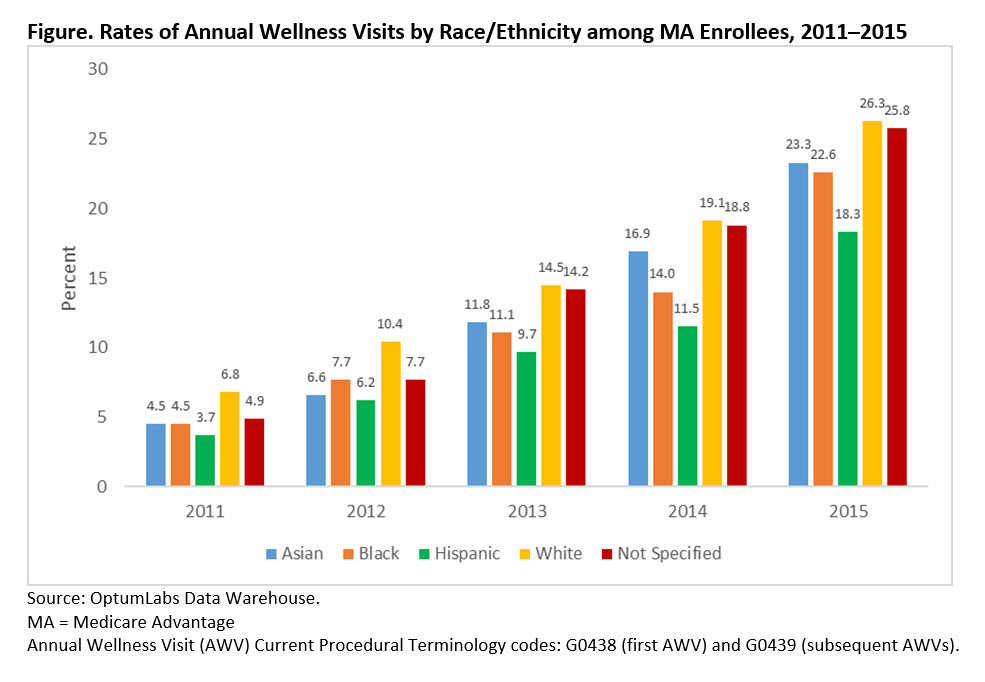
Recently we examined this issue in a study that focused specifically on enrollees in Medicare Advantage (MA), Medicare’s private-plan alternative. Our findings show that about 25 percent of MA enrollees got an Annual Wellness Visit in 2015. A number of factors may contribute to slow uptake across-the-board of the Annual Wellness Visit, such as complexity of documenting, coding, and billing—which may discourage clinicians from recommending this benefit to their patients. On the other hand, lack of access to insurance coverage did not affect our results; the study focused exclusively on enrollees with comprehensive coverage offered by Medicare Advantage plans.
Importantly, we found that minorities were significantly less likely than whites to use this benefit. Our data show that 26 percent of white enrollees got an Annual Wellness Visit, compared to only 22.6 percent of African-American enrollees. The least likely to use the benefit: Hispanic enrollees, at only 18 percent. These trends were consistent throughout the five-year study period.
Among the range of concerns regarding these disparities are the indirect benefits of the Annual Wellness Visit that certain groups may miss. Our study found that people who went for an Annual Wellness Visit were also more likely to get preventive services, like flu and pneumonia vaccinations and cancer screening tests. These disparities raise concerns that those less likely to take advantage of the Annual Wellness Visit might also be less likely to receive preventive services.
Figure. Rates of Annual Wellness Visits by Race/Ethnicity among MA Enrollees, 2011–2015
Our findings echo those of a 2002 Institute of Medicine report that found members of racial and ethnic minorities to be less likely to receive preventive health services as well as often receive lower-quality care and have worse health outcomes for certain conditions. A 2016 follow-up report by the Institute for Health Care Improvement found little progress has been made in reducing disparities since the IOM report.
Sources of Disparities
A variety of reasons could explain the racial and ethnic disparities we found in Annual Wellness Visit use. The American College of Physicians (ACP) has reported that sources of racial and ethnic health care disparities include, among other things, communication difficulties between patient and provider, cultural barriers, provider stereotyping, and lack of access to providers. ACP also reported that minority women are more likely to avoid a doctor’s visit due to cost. In 2018, the Commonwealth Fund reported that unconscious stereotypes and prejudices may create and perpetuate racial and ethnic health disparities. The report suggested that, to combat racial and ethnic disparities, health care professionals must explicitly acknowledge that race and racism factor into health care.
Another study has found lower use of Annual Wellness Visits by non-white beneficiaries in traditional Medicare than other patients in the same practice in 2015. This study also found that half of practices did not provide any Annual Wellness Visits in 2015—suggesting differential availability could be a contributing factor to the disparities we found.
Remedies That Might Work
In an effort to increase overall up-take of Annual Wellness Visits, offering a financial incentive may help. For example, Medicare already has begun to offer beneficiaries a $25 incentive if they receive an Annual Wellness Visit from a Next Generation Accountable Care Organization, an advanced payment model that offers provider groups financial incentives to improve care for Medicare beneficiaries. MA plans could explore adopting similar incentives to encourage enrollees to make use of annual wellness visits and preventive services. Hopefully, this approach would also help narrow the gap in use of annual wellness visits among racial and ethnic groups.
To narrow racial and ethnic disparities in Annual Wellness Visit usage, MA plans may need to adopt targeted measures. Such steps include making sure Hispanic and African-American enrollees are aware of the visit, ensuring they understand it is free, and generally encouraging them to take advantage of it. MA plans could take such steps both through direct consumer communication and provider training and resources (e.g., office literature, etc.). MA plans could provide materials translated into Spanish that describe the annual wellness visit and the benefits of associated preventive services. For instance, the Medicare & You Handbook which described the Annual Wellness Visit is available in Spanish.
In addition, MA plans should ensure that translation services are available to providers (such as through telephone translation services) to ensure they can communicate with patients with limited English proficiency. Also, as suggested by the Commonwealth Fund report above, individual clinicians should make conscious efforts to acknowledge their own biases and treat all enrollees consistently.
Keith Lind is a senior strategic policy adviser at the AARP Public Policy Institute. His areas of expertise include Medicare and chronic care.































































