AARP Hearing Center
New Funding Package Will Improve Access to Care for Older Adults with Depression
By Beth Carter, Claire Noel-Miller, Olivia Dean, March 21, 2023 01:07 PM

One in five people with Medicare — or 12 million individuals — reported symptoms of depression in 2019.1 Moreover, the COVID-19 pandemic only made things worse. In one 2021 survey, 19 percent of older adults reported that their depression or sadness worsened after the onset of the pandemic. Luckily, there is some good news for people with Medicare who suffer from mental health disorders, including those with depression. In December 2022, Congress passed an omnibus funding bill that includes several provisions aimed at improving access to mental health care for Medicare beneficiaries.
Underdiagnosis of Depression Among Older Adults
Despite many Medicare beneficiaries reporting symptoms of depression, the mental illness is often underdiagnosed among older adults. There’s a common misconception that depression is a normal part of aging, so symptoms are often overlooked. Almost half (45%) of people with Medicare report never even being asked about depression by a medical provider. Medicare beneficiaries who report having symptoms of depression are more likely to have had such a conversation, but even among this group, nearly a quarter (24%) had not been asked about depression by a health care professional.1
Barriers to Accessing Care
For many older adults, untreated depression can have significant negative effects — including reduced quality of life, worse health outcomes, and even increased mortality. Many barriers may prevent older adults with depression from getting treatment, including affordability issues, lack of mental health providers, and stigma. In 2019, nearly a quarter of adults ages 50 and older who had a major depressive episode in the previous year reported not being treated for depression. Medicare beneficiaries with depression are also three times more likely to report delaying care due to cost or having difficulty getting needed medical care – which could include mental health care – compared to Medicare beneficiaries without depression (figure).1
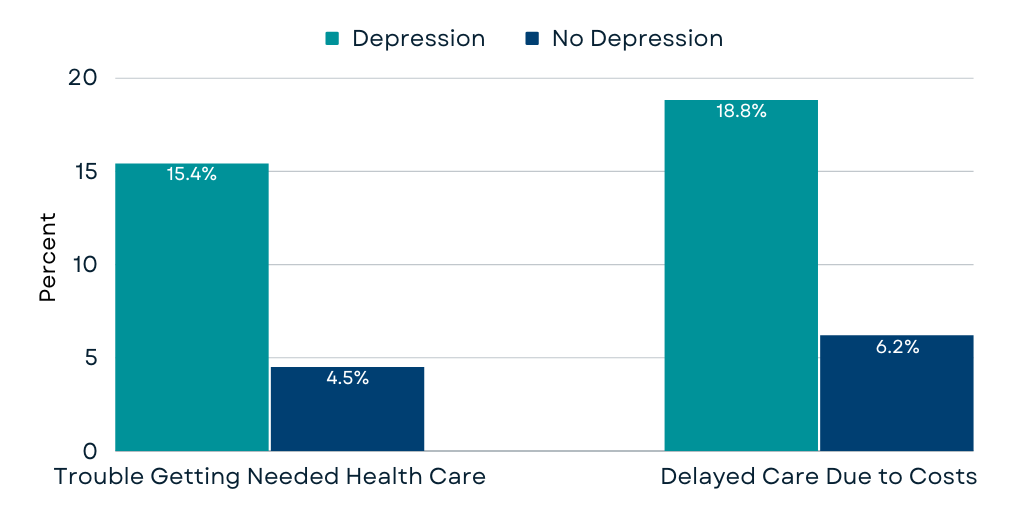
Source: AARP Public Policy Institute’s analysis of the 2019 Medicare Current Beneficiary Survey (MCBS).
Further, although Medicare provides some mental health coverage, the program has some significant gaps, in large part because Medicare isn’t subject to the Mental Health Parity and Addiction Equity Act (MHPAEA) like most other forms of insurance. The MHPAEA requires that coverage for mental health conditions and substance use disorders be comparable to coverage for physical illnesses. In one example of lack of parity, Medicare restricts coverage for inpatient psychiatric hospitals to 190 days during a beneficiary’s lifetime, a limit that does not exist for other Medicare specialty inpatient hospital services. Some people with serious mental illness – including depressive disorders – could quickly surpass this limit.
Recent Funding Package Targets Mental Health Access Barriers
The end-of-year omnibus funding package included provisions that addressed some of the mental health access barriers in Medicare, including expanding the mental health workforce. For example, starting in 2024, licensed mental health counselors (MHCs) and licensed marriage and family therapists (MFTs) will be allowed to bill Medicare for covered mental health services. This could help alleviate the mental health professional shortages that plague many areas of the country. For example, more than half of all counties have no practicing psychiatrists, and there are fewer than 1,300 geriatric psychiatrists nationwide. In contrast, over 190,000 MHCs and MFTs are currently practicing in the United States with an additional 40,000 projected to be in practice by 2030.
The funding package also took steps to improve equitable access to mental health services in Medicare. In a step toward greater parity, the bill requires the Government Accountability Office to conduct a study that compares mental health benefits to other medical benefits in Medicare Advantage (Medicare’s private plan option) and also compares these mental health benefits to those offered in traditional Medicare (also called Original Medicare). In addition, pandemic-related telehealth flexibilities are extended through the end of 2024. These flexibilities have allowed many Medicare beneficiaries who suffer from depression or other mental health illnesses to receive tele-mental health services without a prior in-person visit with their clinician.
Continuing to Address Mental Health Care Access in Medicare
Despite this important progress, more is needed to ensure Medicare beneficiaries with depression have access to the mental health care they need. For one thing, many people with Medicare are not getting some of the mental health services they are eligible for. While Medicare covers one depression screening per year as part of the Annual Wellness Visit, only 6 percent of people with traditional Medicare were screened in 2018.
Further, the demand for mental health care will continue to increase as the number of Americans ages 65 and older is projected to nearly double from 56 million in 2020 to 95 million in 2060. To meet this challenge, policymakers should continue to work to improve Medicare coverage of clinically appropriate mental health services. They should also continue efforts to build a diverse mental health workforce, including those trained in geriatrics, address barriers to diagnosis and treatment, and ensure that older Americans have access to the mental health care they need.
1 Based on AARP Public Policy Institute’s analysis of the 2019 Medicare Current Beneficiary Survey (MCBS).
AARP’s Mental Health Center highlights news and resources for older adults’ mental well-being. If you or someone you know is in immediate emotional distress or in danger of hurting themselves or others, call or text 988 at any time to access free and confidential support and crisis resources.


































































